Cafeteria Plans: Change in Status Events and Permissible Employee Election Changes
Cafeteria plans are governed by IRS Code Section 125 and allow employers to help employees pay for expenses such as health insurance with pre-tax dollars. Employees can choose between a taxable benefit (such as cash) and two or more specified pre-tax qualified benefits (health insurance, for example). Employees can select the benefits they want, much like an individual standing in a cafeteria line.
IRS rules limit the types of benefits that can be offered through a cafeteria plan to:
- Coverage under an accident or health plan (which can include traditional health insurance, health maintenance organizations (HMOs), self-insured medical reimbursement plans, dental, vision, and health flexible spending arrangements (HFSAs)
- Dependent care assistance benefits (DCAPs)
- Group term life insurance
- Paid time off, which allows employees the opportunity to buy or sell paid time off days
- 401(k) contributions (subject to certain restrictions)
- Adoption assistance benefits
- Health savings accounts (HSAs)
Employers cannot offer scholarships, group term life insurance for non-employees, transportation and other fringe benefits, long-term care, and most health reimbursement arrangements (unless very specific rules are met by providing one in conjunction with a high deductible health plan, or certain individual coverage health care arrangements (ICHRAs)). IRS rules also prohibit offering benefits that defer compensation.
Cafeteria plans are not subject to ERISA, but all or some of the underlying benefits or components under the plan can be.
Making Election Changes
Only an eligible employee can make elections, but they can choose benefits that also cover other individuals such as spouses or dependents. Elections, with an exception for new hires and for HIPAA special enrollment periods, must be prospective. Also, cafeteria plan elections are irrevocable and cannot be changed during the plan year, unless a permitted change in status occurs. Note: The IRS has informally stated that mandatory two-year elections for standalone dental or vision plans that meet certain requirements are permitted.
Plans may allow participants to change elections due to:
- Change in legal marital status
- Change in number of dependents
- Change in employment status
- A dependent satisfying or ceasing to satisfy dependent eligibility requirements
- Change in residence
- Commencement or termination of adoption proceedings (only for adoption assistance benefits)
Plans may also allow participants to change elections based on the following changes that are not a change in status:
- Significant cost changes
- Significant curtailment (or reduction) of coverage
- Addition or improvement of benefit package option
- Change in coverage of spouse or dependent under another employer plan
- Loss of certain other health coverage (for example, government provided coverage, such as Medicaid)
- HIPAA special enrollment rights (contains requirements for plans subject to HIPAA)
- Medicare Part D Disclosure
- COBRA qualifying event
- Judgment, decrees, or orders (like qualified medical child support order (QMCSO)
- Entitlement to Medicare or Medicaid
- Family Medical Leave Act (FMLA) leave
- Pre-tax health savings account (HSA) contributions (employees are free to change their HSA contributions whenever they wish, in accordance with their payroll/accounting department process)
- Reduction of hours
- Marketplace enrollment
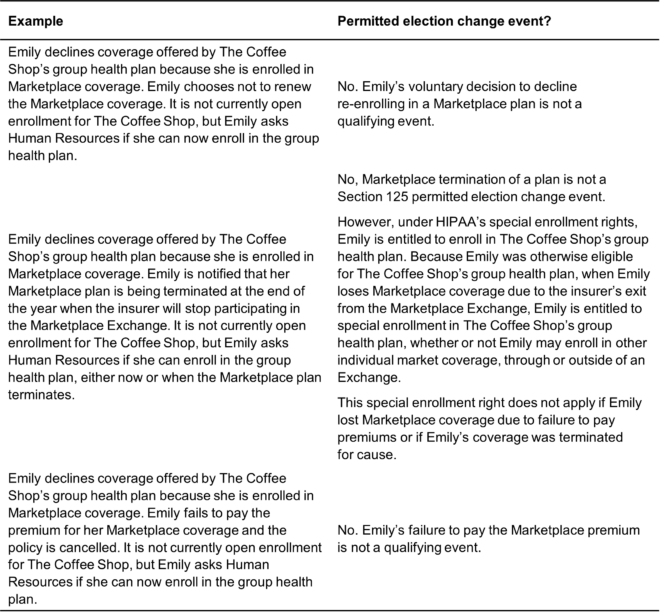
Together, the change in status events and other recognized changes are considered “permitted election change events.”
Common changes that do not constitute a permitted election change event are:
- A provider leaving a network (unless, based on very narrow circumstances, it resulted in a significant reduction of coverage)
- A legal separation (unless the separation leads to a loss of eligibility under the plan), or commencement of a domestic partner relationship
- A change in financial condition
There are some events not in the regulations that could allow an individual to make a mid-year election change, such as a mistake by the employer or employee, or needing to change elections in order to pass nondiscrimination tests. To make a change due to a mistake, there must be clear and convincing evidence that the mistake has been made. For instance, an individual might accidentally sign up for family coverage when they have no children, or an employer might withhold $100 per pay period for a flexible spending arrangement (FSA) when the individual elected to withhold $50.
Plans are permitted to make automatic payroll election increases or decreases for insignificant amounts in the middle of the plan year, so long as automatic election language is in the plan documents. Employers should carefully consider all facts and circumstances when deeming an amount insignificant.
Plans should consider which change in status events to allow, how to track change in status requests, and the time limit to impose on employees who wish to change an election.
Cafeteria plans are not required to allow employees to change their elections; but plans that do allow changes must follow IRS requirements. These requirements include consistency, plan document allowance, documentation, and timing of the election change.
Consistency. In order to make the change, an employee must have experienced the specified change or event, and the requested change must be consistent with the change or event.
Example: Susan is a full-time benefits eligible employee of The Oyster House. Susan becomes Medicare eligible and wishes to make changes to her cafeteria plan elections. If the plan allows, she would be permitted to make changes to any benefit that provides accident or health coverage, including a health FSA. She would not be permitted to make changes to other elections such as dependent care, paid time off, or group life insurance because changing these elections is not consistent with Medicare eligibility.
The consistency rules require that an election change be due to and correspond with the change in status that affects eligibility for coverage under the plan. There are relaxed consistency rules for group term life insurance, dismemberment and disability coverage. There are also special consistency rules for election changes when DCAP or adoption assistance plan expenses are affected; changes due to divorce, death of a spouse or dependent, or a dependent’s loss of eligibility; and a limitation on election changes decreasing or ending coverage because a new family member has become eligible.
DCAP elections cannot be changed because an unemployed individual enrolls in educational courses. If a medical plan automatically terminates dependents when they reach age 26, there would be no qualifying event because no changes would need to be made by the employee.
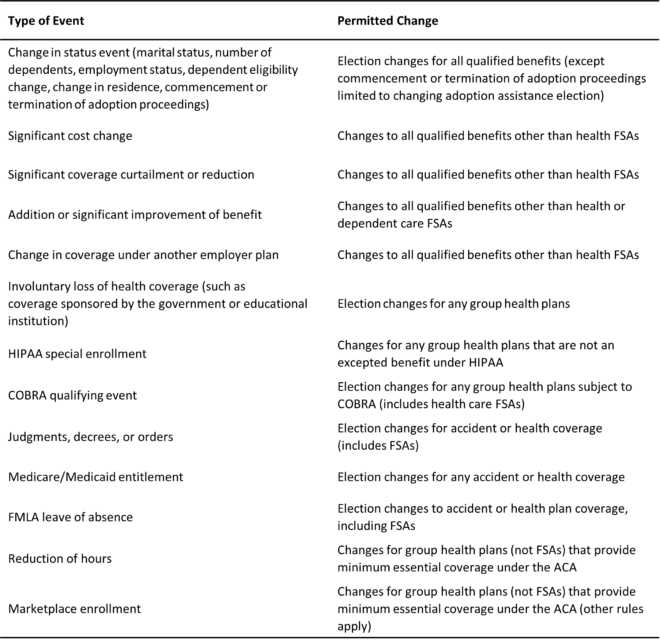
Overview of Consistent Changes
Plan Documents. If an individual has a permitted election change event and the desired change is consistent with the event, but the cafeteria plan document does not recognize the permitted election change event (or the plan does not allow individuals not already on the plan to elect benefits mid-year), the election change is not allowed. If the plan recognizes the change event, not only does the cafeteria plan document have to allow the change, but the plan documents of the component benefit must allow it as well (such as the underlying plan documents for the group health plan).
Documentation and Timing. If the individual has a permitted election change event, the desired change is consistent with the event, and the plan documents allow the change, the plan should document that all requirements have been met. A signed certification by the employee is sufficient. Under ERISA, these records should be kept for at least eight years. Employees are permitted to make changes electronically by self-certifying. The employer should keep electronic records of this change.
Plan administrators should administer election changes involving same-sex spouses in the same manner that they handle election change requests for individuals with opposite-sex spouses.
Change in Status Events
As mentioned above, plans may allow participants to change elections based on an IRS-specified list of change in status events.
Change in Legal Marital Status. Both same-sex and opposite-sex marital status changes are change in status events. Legal separations (unless the legal separation leads to loss of eligibility under the plan) and the commencement and termination of a domestic partnership are not. There is a narrow exception if a domestic partnership changes an individual’s tax status. If a domestic partner qualified as a tax dependent for health coverage purposes, this could trigger a permitted election change event.
Change in the Number of Dependents. The change in the number of dependents can trigger a permitted election change event. Birth, adoption, or placement for adoption will likely trigger a HIPAA special enrollment right, which creates a responsibility for plans subject to HIPAA. “Dependent” refers to a tax dependent under IRS Code Section 152, with an exception for accident and health coverage, under which a child to whom IRS Code section 152(e) applies is treated as a dependent of both parents.
Change in Employment Status. A change in employment status that affects an individual’s eligibility for a benefit is a permissible change in status event. The following events are a change in employment status of an employee (or their spouse, or dependent):
- Termination or beginning of employment
- Strike or lockout
- Return from or start of an unpaid leave of absence
- Change in worksite
If benefits eligibility is dependent upon employment status, and that status changes (such as a move from full time to part-time), this can be a change in status event. However, unless a plan-allowed “reduction in hours or cost change event” occurs when an individual becomes part-time but is still benefits eligible, it is not a qualifying event.
Dependent Satisfying or Ceasing to Satisfy Dependent Eligibility Requirements. If a tax dependent satisfies or ceases to satisfy the requirement for coverage due to aging out, changing student status, marriage, etc., this is a change in status event. Practically speaking, due to the ACA’s requirement to provide health coverage to children under the age of 26, marriage and student status changes are unlikely to trigger a qualifying event for health coverage. This might not be the case for other benefits such as vision or dental coverage.
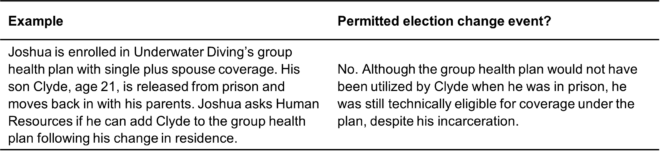
Change in Residence. A change in residence that affects eligibility for coverage would be a permitted election change event. The move must result in a loss of eligibility for coverage. FSAs cannot be changed due to a residence change. If, for example, an individual was covered by an HMO and moved out of the network of providers, the employee could be permitted to drop coverage (if no other coverage was offered by the employer) or elect different coverage.
Commencement or Termination of Adoption Proceedings. For purposes of adoption assistance provided through a cafeteria plan, the commencement or termination of an adoption proceeding is a permitted election change event.
Other Events that Allow a Change in Elections
Outside of the change in status events, the IRS recognizes other events due to which a plan may permit an individual to make an election change.
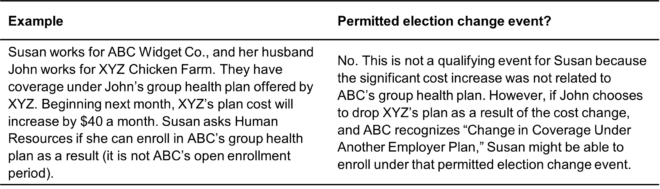
Significant Cost Changes. A plan may permit individuals to make election changes due to significant cost changes. For this rule to apply:
- A benefit plan must be an eligible qualified benefit other than a health FSA.
- The cafeteria plan document must include language regarding significant cost changes.
- For a dependent care assistance plan, the cost change must be imposed by a dependent care provider who is not a relative of the employee.
- The cost change being passed on in the form of changed participant contributions must be significant.
- The plan must determine whether any alternative coverage is similar.
Employees can revoke or drop coverage due to a cost change only if no similar coverage – defined as “coverage of the same category of benefits for the same individuals” – exists. If an employer offers two medical plans, one that is expensive and one that is inexpensive, regardless of the cost change, an employee would only be permitted to switch to the other plan, not revoke coverage entirely. This rule would apply even if the two medical plans were different, such as an HMO versus a high-deductible health plan (HDHP). There is no definition of what constitutes a “significant” cost change, but the change can be employer or employee initiated.
Significant Coverage Curtailment or Reduction. Plans may allow employees to make mid-year election changes due to a significant coverage curtailment, with or without a loss of coverage. The definition of coverage curtailment is not clear, and the regulations state that there is a significant curtailment of coverage “only if there is an overall reduction in coverage provided under the plan so as to constitute reduced coverage generally.”
In the event of coverage curtailment without a loss of coverage, a participant is only permitted to revoke their election and elect similar coverage. If there is a loss of coverage, participants may only revoke elections if “no similar benefits package” is available. Again, if an employer offers two medical plans, the employee would only be permitted to elect the second plan.
Addition or Significant Improvement of Benefit Package Option. If an employer adds a new benefit package option or other coverage option, or if an existing option is significantly improved, eligible employees (including those who had not previously made an election) may revoke their election and make new elections prospectively for coverage under the new plan or option. The term “significant improvement of coverage” is not defined, but generally an increase in medical providers available in network is an improvement. If only one component of the cafeteria plan has an addition, changes can be made only for that component.
Change in Coverage under Another Employer Plan. A cafeteria plan may permit a participant to make election changes due to a change in coverage under another employer plan. This would be triggered if:
- The other employer plan allows a permissible election change.
- The other employer plan has a different period of coverage.
Example: Susan and John each have medical coverage from their respective employers. Susan’s employer has a fiscal year plan; John’s employer has a calendar year plan. Susan and John are married and make no changes to their elections at that time. Six months after getting married they determine that they would like to be on the same plan. Shortly thereafter, Susan’s plan has open enrollment. She drops her employer coverage during open enrollment, thus triggering a permissible change that would allow John to enroll her in his employer’s plan.
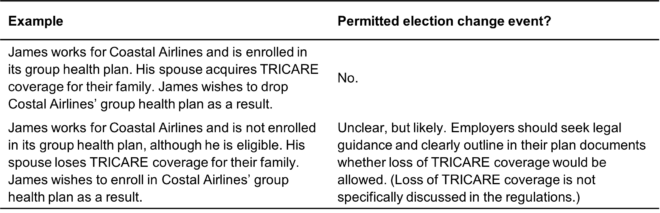
Loss of Group Health Coverage Sponsored by Governmental or Educational Institutions. A plan may allow participants to make changes due to the loss of coverage under other group health coverage, such as a state children’s health insurance program (CHIP), a medical program of an Indian Tribal government, a state health benefits risk pool, or a foreign government group health plan. This change applies only to the loss of coverage. Loss of coverage from an educational institution would also qualify.
HIPAA Special Enrollment Rights. Group health plans subject to HIPAA must provide special enrollment for certain individuals. Plans are not required to allow pre-tax election changes for HIPAA special enrollment events; however, the administrative overhead of handling these changes on an after-tax basis can be burdensome.
HIPAA special enrollment rights overlap with other change in status events. The other events are permissive, but HIPAA enrollment events require the ability to make health coverage changes. HIPAA special enrollment rights also allow a limited ability to elect retroactive coverage on a pre-tax basis. HIPAA special enrollment events also obligate the employer to offer a special enrollment period of a minimum specific duration, typically 30 or 60 days depending on the event.
HIPAA special enrollment events include the loss of health coverage (including loss of eligibility for short-term, limited-duration insurance), acquisition of a new dependent (by marriage, birth, adoption, or placement for adoption) and loss of Medicaid or CHIP coverage.
Enrollment due to loss of coverage under a group health plan means loss of eligibility for non-COBRA coverage, termination of employer contributions toward non-COBRA coverage, or exhaustion of COBRA coverage. It could also apply to the loss of student or private insurance. HIPAA special enrollment events permit employees to add coverage for other dependents at the same time.
Although retroactive elections are typically prohibited, under HIPAA if a newborn or child who is adopted or placed for adoption is enrolled during the special enrollment period, the child can have retroactive coverage to the date of birth, adoption, or placement for adoption.
Medicare Part D Creditable Coverage Disclosure. If an individual was inadequately informed that they never had creditable coverage, the individual may enroll or disenroll in a prescription drug plan at any time.
This is not a cafeteria plan permitted election change event. However, it’s a prescription drug plan election change event under the Medicare Part D creditable coverage disclosure regulations.
COBRA Qualifying Events. A plan may permit an individual to make changes due to COBRA qualifying events. This would allow an individual who became part-time, lost benefit eligibility, and then elected COBRA, to increase salary reductions to pay the increased COBRA cost. This would only be permissible if the individual lost health plan eligibility but not cafeteria plan eligibility. An individual whose child elected COBRA after reaching age 26 could also make a mid-year election change to increase pre-tax deductions to pay for the coverage for the rest of the taxable year.
Judgments, Decrees, and Orders. A plan may allow election changes due to a judgment, decree, or court order, including qualified medical child support orders (QMCSOs). Plan sponsors are not required to allow this change, but not doing so would create a legal conflict if the plan documents and court order are at odds. This exception allows employees to enroll a child in coverage or drop a child from coverage, as ordered by the court. This exception does not include voluntary changes in health coverage between a child’s parents.
Medicare or Medicaid Entitlement. A plan may allow employees to drop or reduce coverage for themselves, their spouse, or dependents, when any of those covered individuals become entitled to Medicare or Medicaid. If an employee drops their coverage under the cafeteria plan, they should consider the impact on their covered spouse’s or dependents’ eligibility under their group plan.
FMLA Leave of Absence. A plan may allow election changes due to leaves of absence under FMLA. FMLA requires covered employers to permit eligible employees to take a certain amount of unpaid job-protected leave. An employer must maintain coverage under any group plan during FMLA leave at the level and under the conditions that would have applied if the individual had not taken FMLA leave. However, a plan may allow an employee to revoke or continue coverage or discontinue employee contributions while on FMLA leave. Upon return from leave, the employee has the right to have coverage reinstated or changed if their coverage was terminated during the leave. (For example, for failure to pay premiums, to add a new child to benefits, or to increase FSA elections.) To pay for the continued coverage, the employee may prepay, make ongoing payments, or make catch-up contributions.
Pre-Tax HSA Contributions. Employees may make changes to HSA contributions through pre-tax salary reductions at any time during the year, as long as the change is effective before the salary to which the change applies becomes available to the employee.
Reduction of Hours. A plan may allow a participant whose hours are reduced below 30 hours a week due to a change in employment status to drop employer-sponsored health coverage mid-year, regardless of whether the hour reduction caused a change in the employee’s eligibility status. IRS rules require that:
- The employee has been in an employment status under which the employee was reasonably expected to average at least 30 hours of service per week and there is a change in that employee’s status so that the employee will reasonably be expected to average less than 30 hours of service per week after the change, even if that reduction does not result in the employee ceasing to be eligible under the group health plan.
- The revocation of the election of coverage under the group health plan corresponds to the intended enrollment of the employee, and any related individuals who cease coverage due to the revocation, in another plan that provides minimum essential coverage with the new coverage effective no later than the first day of the second month following the month that includes the date the original coverage is revoked.
This would allow an employee, otherwise locked into coverage due to the employer’s use of the ACA’s measurement and stability period, to drop coverage during a stability period.
Marketplace Enrollment. The Marketplace enrollment event permits plans to allow participants who are eligible to enroll in Marketplace coverage during a special enrollment period to drop employer-sponsored health coverage mid-year, so long as the employee intends to enroll in Marketplace coverage. The employer only must obtain a reasonable representation from the employee that they intended to enroll on the Marketplace. The following conditions must be met:
- The employee is eligible for a special enrollment period to enroll in a qualified health plan through a Marketplace pursuant to guidance issued by the Department of Health and Human Services and any other applicable guidance, or the employee seeks to enroll in a qualified health plan through a Marketplace during the Marketplace’s annual open enrollment period.
- The revocation of the election of coverage under the group health plan corresponds to the intended enrollment of the employee and any related individuals who cease coverage due to the revocation in a qualified health plan through a Marketplace for new coverage that is effective beginning no later than the day immediately following the last day of the original coverage that is revoked.