Compliance Recap | May 2019
May was a busy month in the employee benefits world. The Internal Revenue Service (IRS) released health savings account annual contribution limits and high deductible health plan minimum annual deductibles and annual out-of-pocket maximums for 2020.
The Department of Labor (DOL) released questions and answers (Q&As) to clarify its enforcement of the association health plan final rule. The Department of Health and Human Services (HHS) published a final rule that implements conscience rights protections contained in federal laws.
The Department of Health and Human Services’ Office for Civil Rights (OCR) released a proposed rule to revise its regulations implementing the Patient Protection and Affordable Care Act’s Section 1557. The IRS released an information letter on how to determine whether an item is a Section 213 medical care expense.
The OCR released a fact sheet clarifying when business associates are directly liable for violations of the Health Insurance Portability and Accountability Act (HIPAA). The OCR also released frequently asked questions regarding HIPAA liability when an app uses or discloses protected health information.
IRS Releases 2020 HSA Contribution Limit and HDHP Deductible Minimum and OOP Maximum
The Internal Revenue Service (IRS) released the annual contribution limits for health savings accounts (HSAs) and the high deductible health plan (HDHP) minimum annual deductibles and the HDHP annual out-of-pocket (OOP) maximums for the 2020 calendar year.
The HSA contribution limit will be $3,550 for self-only coverage and $7,100 for family coverage. The HDHP minimum annual deductible will be $1,400 for self-only coverage and $2,800 for family coverage. The HDHP OOP maximum will be $6,900 for self-only coverage and $13,800 for family coverage.
Update on DOL Enforcement Policy Regarding Association Health Plans
On March 28, 2019, the U.S. District Court for the District of Columbia (Court) found that the Department of Labor (DOL) association health plans (AHPs) final rule exceeded the statutory authority delegated by Congress under the Employee Retirement Income Security Act (ERISA) and that the final rule unlawfully expands ERISA’s scope. In particular, the Court found the final rule’s provisions – defining “employer” to include associations of disparate employers and expanding membership in these associations to include working owners without employees – were unlawful and must be set aside.
On May 13, 2019, the DOL issued Questions and Answers – Part Two (Q&As) as follow up to the DOL’s April 2019 AHP enforcement statement. In the Q&As, the DOL clarifies two points.
First, although new AHPs formed under the DOL’s final rule cannot market to and sign up new employer members, existing AHPs can continue to enroll new employees upon HIPAA special enrollment events (for example, upon marriage, birth, adoption, placement for adoption, or loss of eligibility for other coverage) and consistent with the plan’s eligibility terms (for example, enrolling new hires) while the DOL’s enforcement relief remains in effect.
Second, although AHPs are not required to obtain an advisory opinion from the DOL, AHPs with questions about whether they meet the DOL’s pre-rule guidance for sponsoring an AHP can either request an official advisory opinion from the DOL or have an informal discussion with the DOL’s employee benefits law specialists by contacting the DOL.
In the upcoming months, the U.S. Court of Appeals for the District of Columbia Circuit will consider the legal arguments in this case. Employers in AHPs should keep apprised of future developments in this case.
Read more about the DOL’s enforcement of the final rule.
HHS Publishes Conscience Rights Final Rule
On May 21, 2019, the Department of Health and Human Services (HHS) published a final rule and released a fact sheet to implement the conscience rights protection provisions contained in federal laws such as the Church Amendments, the Coats-Snowe Amendment, the Weldon Amendment, and the Patient Protection and Affordable Care Act (ACA).
Although the final rule does not create any new conscience rights protection, individuals, health care entities (including health plans and plan sponsors), and providers are protected from discrimination in health care (based on their religious belief or moral conviction) by government or government-funded entities. The final rule requires applicants for and recipients of federal financial assistance from HHS to attest that they will comply with conscience rights and anti-discrimination laws. The final rule implements enforcement tools, such as investigating complaints, compliance reviews, and withholding federal funds, similar to other civil rights laws, to ensure compliance with federal conscience rights protection laws.
OCR Releases Proposed Rule to Revise ACA Section 1557 Regulations
The Department of Health and Human Services’ Office for Civil Rights (OCR) released a proposed rule and fact sheet to revise its regulations under the Patient Protection and Affordable Care Act’s Section 1557. The current Section 1557 regulations remain in effect until a final rule is published.
The proposed rule would eliminate:
- Certain definitions, including the definition of “covered entity”
- Specific nondiscrimination definitions based on sex and gender identity
- Translated taglines in significant consumer communications, the requirement to post information about Section 1557 and nondiscrimination at a covered entity’s locations and website, use of language access plans, and certain video standards for individuals with limited English proficiency (LEP)
- Any reference to a private right of action to sue covered entities for violations of the proposed rule
- The requirement to have a compliance coordinator and written grievance procedure to handle complaints about Section 1557 violations
- Enforcement-related provisions
Public comment on this proposed rule will close 60 days after the proposed rule is published in the Federal Register. After considering public comments, OCR will issue a final rule. The final rule will be effective 60 days after it is published in the Federal Register.
Read more about the proposed rule in our Updated on Nondiscrimination Regulations Relating to Sex, Gender, Age, and More Advisor and our Update on Nondiscrimination Regulations Relating to Sex, Gender, Age, and More – for Health Care Providers Advisor.
IRS Releases Information Letter on Section 213 Medical Care Expenses
The Internal Revenue Service (IRS) released an information letter in response to a question of whether menstrual care products’ costs qualify as medical care expenses under Internal Revenue Code Section 213 for purposes of health savings accounts, health flexible spending accounts, and other tax-preferred accounts.
Although the IRS declined to specifically answer the question, it indicates that medical care expenses under Section 213 are limited to expenses paid primarily for the prevention or alleviation of a physical or mental defect or illness. Generally, an expense that benefits a person’s general health is a personal expense and not a medical care expense. A personal expense will only qualify as a medical care expense if the person would not have incurred the expense but for the person’s disease or illness.
The IRS lists some objective factors to use in determining whether an expense may qualify as a Section 213 medical care expense:
- The motive or purpose for making the expenditure
- A medical condition diagnosis and a physician’s recommendation of the item as treatment or mitigation
- The relationship between the treatment and the illness
- The treatment’s effectiveness
- The proximity in time to the disease’s onset or recurrence.
OCR Releases Fact Sheet on Business Associate Liability
The Department of Health and Human Services Office of Civil Rights (OCR) recently released a fact sheet listing ten HIPAA violations for which business associates are directly liable.
OCR Releases FAQs on HIPAA Applicability to Health-Related Apps
The Department of Health and Human Services Office for Civil Rights (OCR) recently released five Access Rights, Apps and APIs frequently asked questions (FAQs) regarding covered entities’ liability under HIPAA and HITECH for an application’s (app) use or disclosure of an individual’s protected health information (PHI).
If the app is not provided by or on behalf of the covered entity, the covered entity will not be liable for a PHI breach experienced by the app. However, if the app was developed for or provided by or on behalf of the covered entity, the covered entity could be liable under HIPAA because the app developer would be a business associate. A covered entity will not be liable for a PHI breach that occurs due to a person’s request that unencrypted PHI be transmitted to an app.
Question of the Month
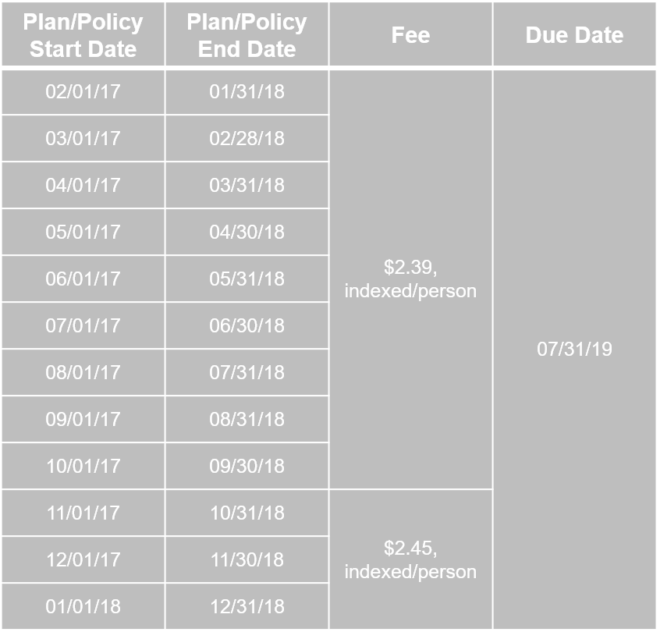
- Who must pay the Patient-Centered Outcomes Research Institute (PCORI) fee and when is the fee due?
- The fee must be determined and paid by:
- The insurer for fully insured plans (although the fee likely will be passed on to the plan)
- The plan sponsor of self-funded plans, including HRAs
- The plan’s TPA may assist with the calculation, but the plan sponsor must file IRS Form 720 and pay the applicable fee
- If multiple employers participate in the plan, each must file separately unless the plan document designates one as the plan sponsor
The fee is due by July 31, 2019 for the following plan/policy years: