Health Savings Accounts: What You Need to Know
A health savings account (HSA) is a tax-exempt trust or custodial account set up with a qualified HSA trustee (such as a bank or insurance company) that is used to pay or reimburse certain medical expenses.
HSAs were first available as of January 1, 2004, and have grown greatly in popularity. An eligible individual (with or without employer involvement) can establish an HSA. Eligible participating individuals can make contributions, up to statutory limits, and get a tax deduction. Investment earnings on HSA accounts are tax free, and HSA funds used to pay qualified medical expenses are completely tax free. Employers contributing to their eligible employees’ HSAs, or that offer HSAs through a cafeteria plan also receive federal tax deductions for the contributions.
Because of these benefits, HSAs are highly regulated; by Internal Revenue Code Section 223, as well as numerous IRS notices and guidance documents. IRS Publication 969 provides a basic overview of HSA regulations for employers and employees.
In response to the spread of the 2019 Novel Coronavirus (COVID-19), on March 11, 2020, the IRS released a notice regarding HSA-qualified high deductible health plan (HDHP) coverage of testing and treatment related to COVID-19. Under the notice, health plans that otherwise qualify as HSA-eligible HDHPs will not lose that status solely because they cover the cost of testing for or treatment of COVID-19 before the plan’s minimum deductible has been met. The notice provides that vaccinations continue to be considered preventive care and can be paid for by the HDHP without first meeting a deductible.
The following provides a summary of the HSA rules.
Eligibility
To be an eligible individual and qualify for an HSA, you must meet the following requirements.
- You must be covered under a high deductible health plan (HDHP) on the first day of the month.
- You have no other disqualifying health coverage except what is
- You are not enrolled in
- You cannot be claimed as a dependent on someone else’s tax return for the
High Deductible Health Plan
To participate in an HSA, an individual must be covered under an HDHP on the first day of the month.
The HDHP must provide “significant benefits.” For example, it cannot exclude in-patient care or hospitalizations, be a fixed indemnity benefit, or only cover certain specified diseases such as cancer.
In 2021, the individual must have an annual deductible of at least $1,400 for self-only coverage ($1,400 for 2022), and the deductible and out-of-pocket expense cannot exceed $7,000 ($7,050 for 2022). These dollar figures change annually. For an individual enrolled in family coverage (or, other than self-only), the deductible must be at least $2,800 in 2021 ($2,800 for 2022), and the deductible and out-of-pocket expenses cannot exceed $14,000 ($14,100 for 2022).
Generally, an HDHP may not provide benefits for any year until the minimum deductible for that year is satisfied. However, there’s a safe harbor that allows an HDHP to have no deductible for preventive care, in part because the Patient Protection and Affordable Care Act (ACA) requires non-grandfathered group health plans and issuers to provide benefits for certain preventive health services without imposing cost-sharing requirements.
Before July 17, 2019, the definition of preventive care generally did not include any service or benefit intended to treat an existing illness, injury, or condition.
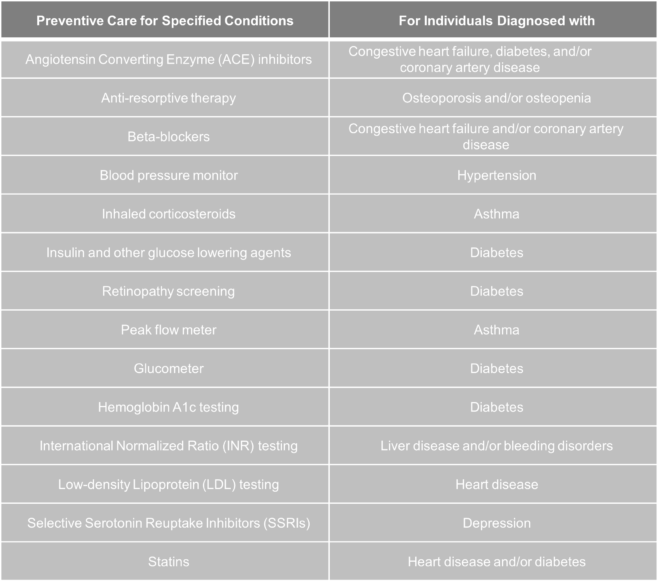
Effective July 17, 2019, the IRS expanded the list of preventive care benefits that an HDHP can provide without a deductible or with a deductible below the annual minimum deductible:
The services and items listed above are treated as preventive care:
- only when prescribed to treat a person diagnosed with the associated chronic condition listed in the table’s second column, and
- only when prescribed for the purpose of preventing the chronic condition’s exacerbation or a secondary condition’s development.
If a person is diagnosed with more than one chronic condition, all listed services and items applicable to the multiple conditions are preventive care.
Other Disqualifying Coverage
In addition to the requirement that an individual be enrolled in an HDHP, an HSA eligible individual cannot have other disqualifying coverage.
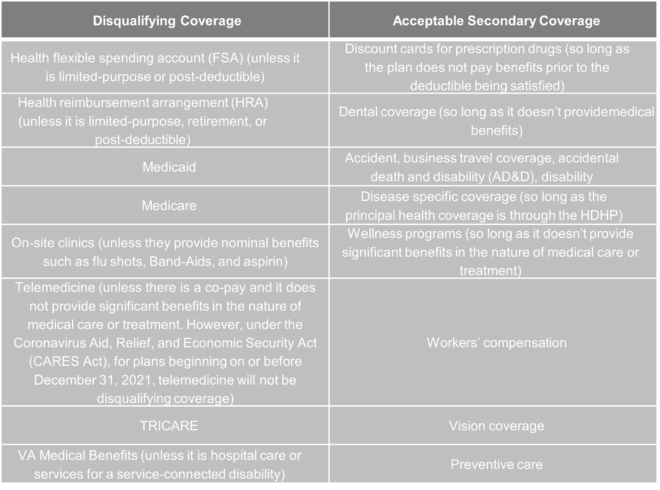
Example: Adam and Susan are married; Adam is a full-time employee at The Auto Dealer and enrolls in its HDHP. Susan is a full-time employee at The Dry Cleaner and enrolls in its HMO plan with an FSA. Both Adam and Susan enroll in single-only coverage. Because Susan now has an FSA, which the IRS allows her to spend on Adam even if she has single-only coverage, Adam is no longer HSA eligible because he is now covered by disqualifying coverage (even if Susan does not spend any of the FSA on Adam’s qualifying expenses). If Susan chose to enroll in The Dry Cleaner’s limited purpose FSA instead of the general-purpose FSA, Adam could maintain his HSA eligibility.
Interplay Between Health FSAs and HSAs
Special issues can arise when an employer offers multiple benefit plans, including a traditional health plan with an FSA account, and an HDHP with an HSA account. These same issues arise when an employer looks to change the benefit plan it offers from a traditional plan with an FSA and an HDHP with an HSA.
When an individual has an FSA, they have coverage that disqualifies them from being HSA eligible. The question becomes, when are they considered to have “dropped” the FSA in order to gain HSA eligibility? The answer is different depending on the FSA’s plan design and whether the individual has a remaining balance at the end of the plan year.
Health FSA with a Grace Period
Some cafeteria plans allow participants to access unused FSA funds for a period up to 2.5 months after the close of the plan year. The grace period is a time during which additional reimbursable expenses can be incurred. An FSA with a grace period cannot allow carryovers (see below). Guidance issued in 2020 and 2021 to address FSA issues arising from the COVID-19 global pandemic increased grace periods for plans that are amended by December 31, 2021. Employers who make these amendments should be aware that doing so will further delay an individual’s ability to contribute to an HSA.
- Participant has unused balance at the end of the year, and FSA has a grace period.
- Participant is not eligible for an HSA contribution until the first calendar month beginning after the grace period ends.
- Participant has no year-end balance, and FSA has a grace period.
- Participant becomes HSA eligible at the end of the FSA plan year, including during the grace period. This requires a $0 balance in the FSA.
Health FSA with Carryovers
FSAs are now allowed to offer carryovers of unused balances of up to $500 remaining at the end of the plan year, to be used for qualified medical expenses for subsequent plan years. An FSA with a carryover cannot have a grace period (see above). Guidance issued in 2020 and 2021 to address FSA issues arising from the COVID-19 global pandemic increased eligible carryover amounts for plans that are amended by December 31, 2021. Employers who make these amendments should be aware that doing so will further delay an individual’s ability to contribute to an HSA.
- Participant has a general-purpose FSA with a carryover provision.
- Regardless of whether or not the FSA funds are exhausted prior to the end of the plan year, the individual is ineligible to participate in an HSA for the entire subsequent plan year.
- Participant has a general purpose FSA with a carryover provision, but the plan allows employees to decline or waive their carryovers at the beginning of the next plan year.
- If the participant declines or waives the carryover (regardless of the amount of funds in the FSA), he or she becomes eligible for an HSA at the end of the FSA plan year.
- Participant has a general-purpose FSA with funds remaining but is allowed to carry over the unused amount into a limited-purpose FSA.
- If the participant carries unused funds over into a limited- purpose FSA, he or she becomes eligible for an HSA at the end of the FSA plan year.
Medicare
Being entitled to Medicare makes a person ineligible for an HSA, even if the person is enrolled in a qualifying HDHP.
Internal Revenue Code (IRC) Section 223 reads: “Medicare eligible individuals. The [contribution limit] under this subsection for any month with respect to an individual shall be zero for the first month such individual is entitled to benefits under title XVIII of the Social Security Act and for each month thereafter.”
Being eligible for and being entitled to Medicare are not the same. A person becomes eligible for Medicare through age, through disability, or due to end stage renal disease (ESRD).
Individuals are entitled to Medicare once they are 65 years old and they either have applied for and are receiving benefits from the Social Security or Railroad Retirement Board, or are eligible for monthly retirement benefits from Social Security or the Railroad Retirement Board (but have not applied for them) but have filed an application for Medicare Part A.
For a person who is working and aged 65 or over to maintain HSA eligibility he or she must:
- Not apply for or waive Medicare Part A, and
- Not apply for Medicare Part B, and
- Waive or delay Social Security
When employment-related coverage ends, a person has eight months to enroll in Medicare Part A, which, once effective, will be effective for six months retroactively, but no earlier than the first day of eligibility.
This means that if a person maintained HSA-eligibility (by waiving or delaying Social Security benefits, waiving or not applying for Medicare Part A, and not applying for Medicare Part B), then the person should stop making HSA contributions six months before enrolling in Part A and B (or before applying for Social Security benefits) because, in most cases, a person’s Medicare coverage will be retroactive up to six months from the time the person enrolls in Medicare.
Because a person’s Medicare coverage would be retroactive, the Medicare coverage would be HSA- disqualifying coverage. That’s why a person who has maintained HSA eligibility after reaching age 65 should, in most cases, stop making HSA contributions six months before enrolling in Part A and B (or before applying for Social Security benefits).
Dependent Status
Individuals who can be claimed as a dependent on someone else’s tax return are not HSA eligible.
Example: Anna is 15 years old and is claimed as a dependent on her parent’s taxes. Her mom, Caroline, has enrolled in family HDHP coverage through her employer and has established an HSA to which she can contribute up to the full family amount. Anna does not have any other disqualifying coverage, but she cannot establish an HSA because she is claimed as a dependent on her parent’s taxes.
Another complicated wrinkle in dependent status and HSAs involves whose expenses can be reimbursed from the HSA. HSAs can only reimburse the expenses of the employee, spouse, and tax dependents as defined by IRS Code Section 223(d)(2)(A) (even if the person is not eligible to set up his or her own HSA) if the expense was incurred after the HSA is established.
Example: Samuel is 24 years old and is not claimed as a dependent on his parent’s taxes. His mom, Caroline, has enrolled in family HDHP coverage through her employer (which covers Samuel) and has established an HSA into which she can contribute up to the full family amount. Samuel does not have any other disqualifying coverage, and he can establish his own HSA (although his employer is unlikely to allow him to put pre-tax dollars into it). Caroline cannot spend her HSA dollars on Samuel’s medical expenses, even though he is covered under the family HDHP. That is because Samuel is not a tax dependent of his parent.
Determining Eligibility; Changes in Eligibility
An individual’s eligibility is determined monthly, on the first day of the month.
If an individual is enrolled in single HDHP coverage on the first day of September (and has no disqualifying coverage), the individual is eligible to contribute up to the full single contribution limit for the month (1/12 of the annual limit) of September, as well as October, November, and December. If an individual enrolls on the 15th of September in single HDHP coverage (and has no disqualifying coverage), the individual can begin contributing up to the full single contribution limit for the months of October, November, and December, but not the month of September. That is because the individual was not HSA eligible on the first day of September. If an individual changes from family to single coverage, or vice versa, the limit for that month is based on the individual’s coverage as of the first day of the month.
Contribution
The amount you or any other person can contribute to your HSA depends on the type of HDHP coverage you have, your age, the date you become an eligible individual, and the date you cease to be an eligible individual. For 2021, if you have self-only HDHP coverage, you can contribute up to $3,600 ($3,650 for 2022). If you have family HDHP coverage, you can contribute up to $7,200 for 2021 ($7,300 for 2022).
The “last-month” rule also provides that individuals who are eligible for an HSA on December 1 (the last month of the year), are considered eligible for the entire year. The individual is considered to have the HDHP coverage on December 1 for the entire year.
If an individual changes from family to single coverage during the year, the individual’s maximum contribution amount is calculated as (X/12 x $7,200) + (Y/12 x $3,600) = $ . The dollar figures used in the formula will change annually based on the IRS contribution limits.
X represents the number of months the individual was eligible under family coverage; Y represents the months the individual was eligible for single coverage.
Individuals who reach age 55 by the end of the taxable year have their contribution limit increased by $1,000, regardless of the tier of coverage they are enrolled in. This is called a “catch-up” contribution. A married couple, both age 55 or older, can make two catch-up contributions, but there must be a separate HSA for each spouse. Because HSAs are individual trusts, spouses cannot have a joint HSA (but each spouse can spend his or her individual HSA dollars on the spouse’s medical expenses).
The IRS has a “special rule” for married individuals that allows a couple to divide the maximum HSA contribution between spouses so long as one of them has family HDHP coverage, and neither has disqualifying coverage. The IRS provides the following example:
For 2021, Mr. Auburn and his wife are both eligible individuals. They each have family coverage under separate HDHPs. Mr. Auburn is 58 years old and Mrs. Auburn is 53. Mr. and Mrs. Auburn can split the family contribution limit ($7,200) equally or they can agree on a different division. If they split it equally, Mr. Auburn can contribute $4,600 to an HSA (one-half the maximum contribution for family coverage ($3,600) + $1,000 additional contribution) and Mrs. Auburn can contribute $3,600 to an HSA.
Beginning the first month an individual is enrolled in Medicare (or entitled to Medicare) the contribution limit is zero.
Example: Marie turned age 65 in July 2020 and enrolled in Medicare. She had an HDHP with self-only coverage and is eligible for an additional contribution of $1,000. Her contribution limit is $2,275
($4,550 × 6 ÷ 12).
If an individual makes contributions in excess of the IRS annual limits, he or she must pay a 6 percent excise tax on the excess contributions, and the excise tax will apply to each year the excess contribution remains in the individual’s account. The excise tax is paid with IRS Form 5329.
Employer Contributions
Employers may contribute to an employee’s HSA, but their contributions count toward the individual’s total contribution limit for the year.
One of two sets of nondiscrimination rules applies to HSA contributions from employers. If the employer makes contributions through a Section 125/cafeteria plan, the contributions are included in the plan’s cafeteria plan nondiscrimination testing. These rules generally prohibit employers from favoring highly compensated or key employees.
Comparable contributions. If the employer does not include the HSA in its Section 125/cafeteria plan, it is subject to the comparable contributions rule.
In this case, if an employer makes contributions, it must make comparable contributions to all comparable participating employees’ HSAs. Contributions are comparable if they are either:
- The same amount, or
- The same percentage of the annual deductible limit under the HDHP covering the employees.
This rule prohibits employers from implementing HSA “matching” programs or using HSA contributions as a wellness incentive.
Comparable participating employees:
- Are covered by their HDHP and are eligible to establish an HSA,
- Have the same category of coverage (either self-only or family coverage), and
- Have the same category of employment (part-time, full-time, or former employees).
Distributions
Individuals may receive tax-free distributions from their HSA to pay or be reimbursed for qualified medical expenses incurred after the establishment of the HSA. If an individual loses HSA eligibility at any point, he or she can continue to spend remaining HSA dollars on qualified medical expenses.
HSA-qualified expenses are all medical expenses allowed by IRC Section 213, except insurance premiums (unless for COBRA, long-term care insurance, or any deductible health insurance if the HSA holder is 65 or older (not including a Medicare supplemental policy), which may be reimbursed). If you use HSA funds to pay premiums for COBRA, long-term care insurance, or Medicare supplement coverage, you cannot claim the health coverage tax credit for those premiums.
A qualified medical expense incurred overseas may be paid with an HSA. Care should be taken to ensure the expense is documented and meets the requirements under IRC Section 213.
Non-prescription or over-the-counter (OTC) medications other than insulin are not considered a qualified medical expense, unless you have a prescription for it. For example, if your physician wrote you a prescription for aspirin or pre-natal vitamins, you could purchase them over the counter with your HSA funds. However, under the CARES Act, OTC medications without a prescription are considered qualifying medical expenses for expenses incurred and amounts paid after December 31, 2019.
Also, under the CARES Act, menstrual care products are categorized as qualified medical expenses for expenses incurred and amounts paid after December 31, 2019.
Qualified medical expenses are those incurred by the following persons.
- You and your spouse
- All dependents you claim on your tax return
- Any person you could have claimed as a dependent on your return except if:
- The person filed a joint return,
- The person had gross income of $4,300 (adjusted for inflation) or more, or
- You, or your spouse if filing jointly, could be claimed as a dependent on someone else’s return.
A child of parents who are divorced (or separated or living apart for the last six months of a calendar year) are treated as the dependents of both parents, regardless of whether the custodial parent releases the claim to the child’s exemption.
HSAs also have prohibited transactions, including the lending of money between the individual and the HSA. This means that, if an individual overdraws the HSA account (which is considered lending money), the individual loses HSA eligibility for the entire year, and will be subjected to an additional 20 percent excise tax. Federal law will require the bank operating the HSA to close it, and the individual cannot reopen the account at that bank, or any other bank, for the entire year.
HSA holders are obligated to keep sufficient records to show that any distributions from their HSA were used exclusively to pay or reimburse qualified medical expenses, that the expense was not paid previously or from another source, and that the individual did not take the expense as an itemized deduction in any year.
Published 7/5/2018
Updated 5/28/2019, 7/18/2019, 3/11/2020, 4/5/2020, 7/30/2020, 8/12/2020, 9/7/2021