Please review the below information to better equip you for your upcoming renewal , as well as ensure that you stay on top of compliance requirements as a small group employer with under 50 employees. If you have any questions after reviewing this information, please reach out to your Brinson Benefits Account Executive.
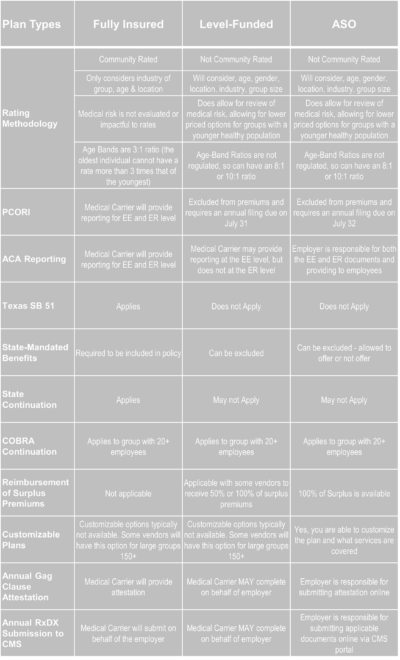
Comparison of Plan Types
Review the below as you prepare for your renewal and learn the differences between fully insured plans and level-funded plans with a self-funded contact. There are some additional requirements when your plan is on a self-funded contract vs. being fully insured.
Health Plan Limits
Review how limits will be changing for the upcoming calendar year and the potential impact to you and your employees.
Annual Notices
Employers that sponsor group health plans are required to provide certain benefit notices on an annual basis. These notices can coincide with your plan renewal or during a set time period each year. Please read more to review the notices and determine which ones apply to you.
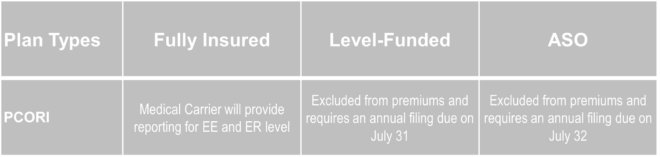
Patient Centered Outcomes Research Institute (PCORI) Fee
This annual fee applies to all employers who offer a Level Funded Plan, Minimum Essential Coverage plan, or a Health Reimbursement Arrangement.
Play or Pay
The Affordable Care Act implemented a penalty for large employees (51+ full time equivalent employees) for not offering a minimal essential health coverage plan to their employees. Please review and prepare if your business will be growing in the coming months.
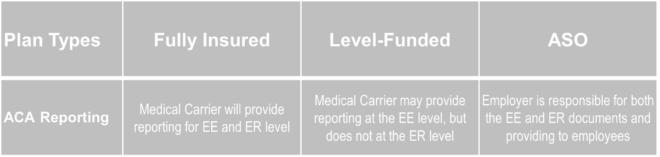
ACA Reporting
Employers providing health coverage may be required to provide specific information to the IRS about individuals offered/covered by their group health plan, as well as provide a statement to their covered employees. Please review to see if you are impacted by this IRS requirement.
Senate Bill 51 (SB51)
This Texas legislation requires for employers to have timely termination of employees within the medical carrier systems. Please read more to learn about this legislation and the guidelines you need to follow to avoid incurring additional premium costs.
RxDC Annual Reporting
Self-funded and level-funded plan sponsors are required to submit annual prescription drug data collection (RxDC) reports as part of the Consolidated Appropriations Act, 2021 (CAA). These reports must be filed electronically via CMS’s HIOS portal by June 1 each year.